Vitamin D deficiency is incredibly common, and supplementing with vitamin D has become increasingly popular. Yet most of the conversation around vitamin D deficiency is about supplementation, which doesn’t address the actual root causes.
So what are the REAL root causes of vitamin D deficiency?
Let’s briefly dive into how vitamin D is metabolized in your body…
Vitamin D Metabolism: Starts with Cholesterol in Your Skin + Sunshine
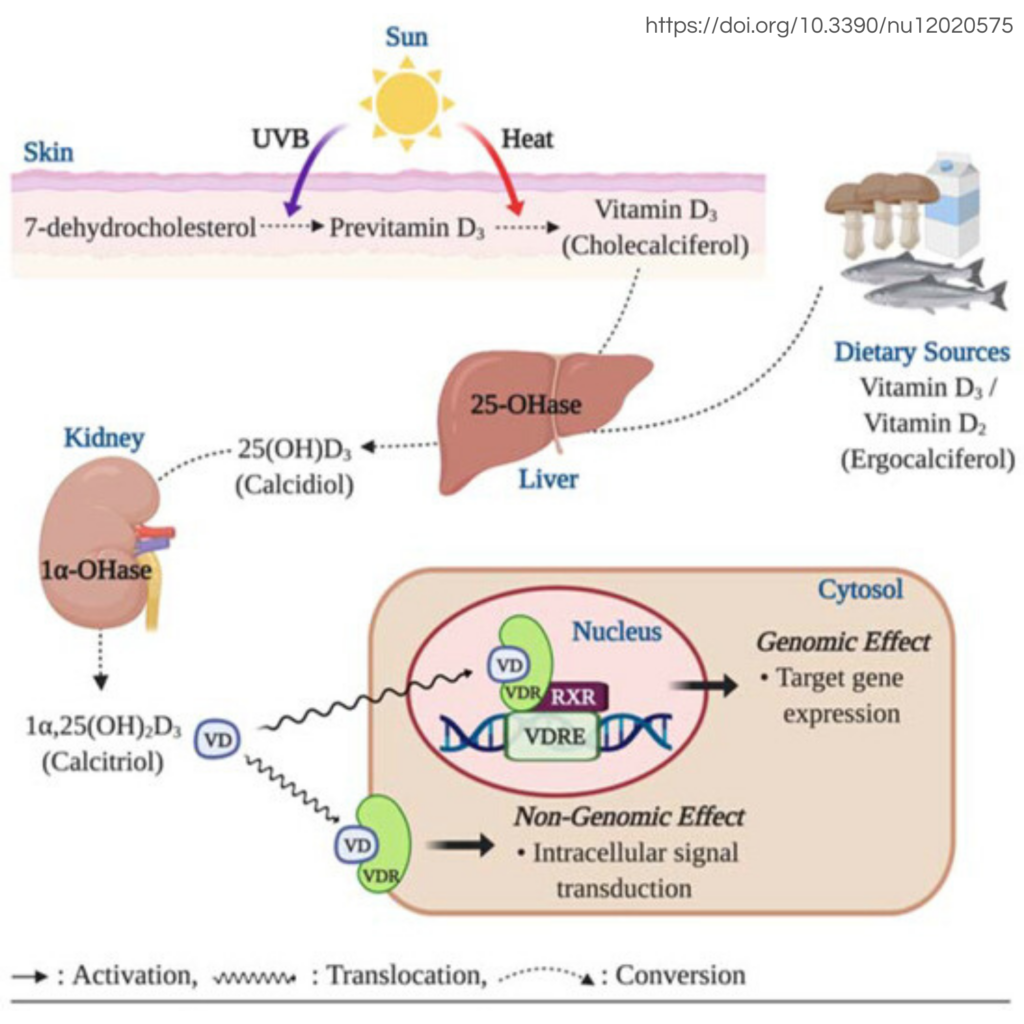
Vitamin D3 (cholecalciferol) is made in the skin from 7-dehydrocholesterol (a cholesterol precursor) in the presence of sunlight. Without adequate exposure to sunlight, vitamin D levels will naturally be lower than optimal. While you can also get a small amount of vitamin D from your diet, sun exposure is where you get most of it.
What impacts UV production of vitamin D? Sunscreen and clothing block vitamin D synthesis, so regular unprotected sun exposure in moderate amounts is necessary and healthy. Also, people who live in higher latitudes will have fewer days of sunshine and therefore less vitamin D production during those cloudy months. However, vitamin D is a fat-soluble ‘vitamin’ (it’s not actually a vitamin, but rather a hormone) which can be stored in fat cells. This is why healthy summer sun exposure is so essential: the vitamin D synthesized during the summer can last you throughout the winter even without supplementation.
Are You Vitamin D Deficient Even Though You Get Plenty of Sun Exposure?
When I was in naturopathic medical school, I learned that you needed to supplement vitamin D levels below 30 ng/mL, with a certain number of IU per every desired 10 ng/mL increase in serum 25-OH vitamin D.
While supplementing could be helpful, vitamin D levels wouldn’t always rise with supplementation or they would fall back to sub-optimal levels once supplementation was discontinued. I also always wondered how people who lived in sunny climates and were always outdoors could be vitamin D deficient, since vitamin D production starts with sun exposure on your skin.
So the sun is needed for vitamin D production, and obviously a lack of time spent out in the sunshine can trigger low levels. But what about for those people who get plenty of healthy sun exposure?
The Role of Your Liver & Kidneys in Vitamin D Metabolism
After it’s synthesized in your skin, vitamin D3 (cholecalciferol) is then converted to 25-OH-D3 in the liver (the form that is often measured in the blood). Then it’s up to your kidneys to convert it to its active form, 1,25-OH-D3. Vitamin D MUST be converted to its active form, 1,25-OH-D3, in order to have its beneficial effects, like calcium regulation and immune system modulation.
Low levels of 25-OH vit D can mean something is up with your liver and/or kidney function. While a number of diseases can affect the liver and kidneys, you can also have subclinical liver or kidney function impairment that may not even be identifiable by common lab markers.
Take insulin resistance for example: you can start to exhibit tendencies toward insulin resistance, blood sugar dysregulation, and metabolic dysfunction before your labs even show high blood sugar levels, and this can definitely affect the health of your liver & kidneys, and ultimately vitamin D metabolism and immune health.
Here are some common causes of liver and kidney dysfunction:

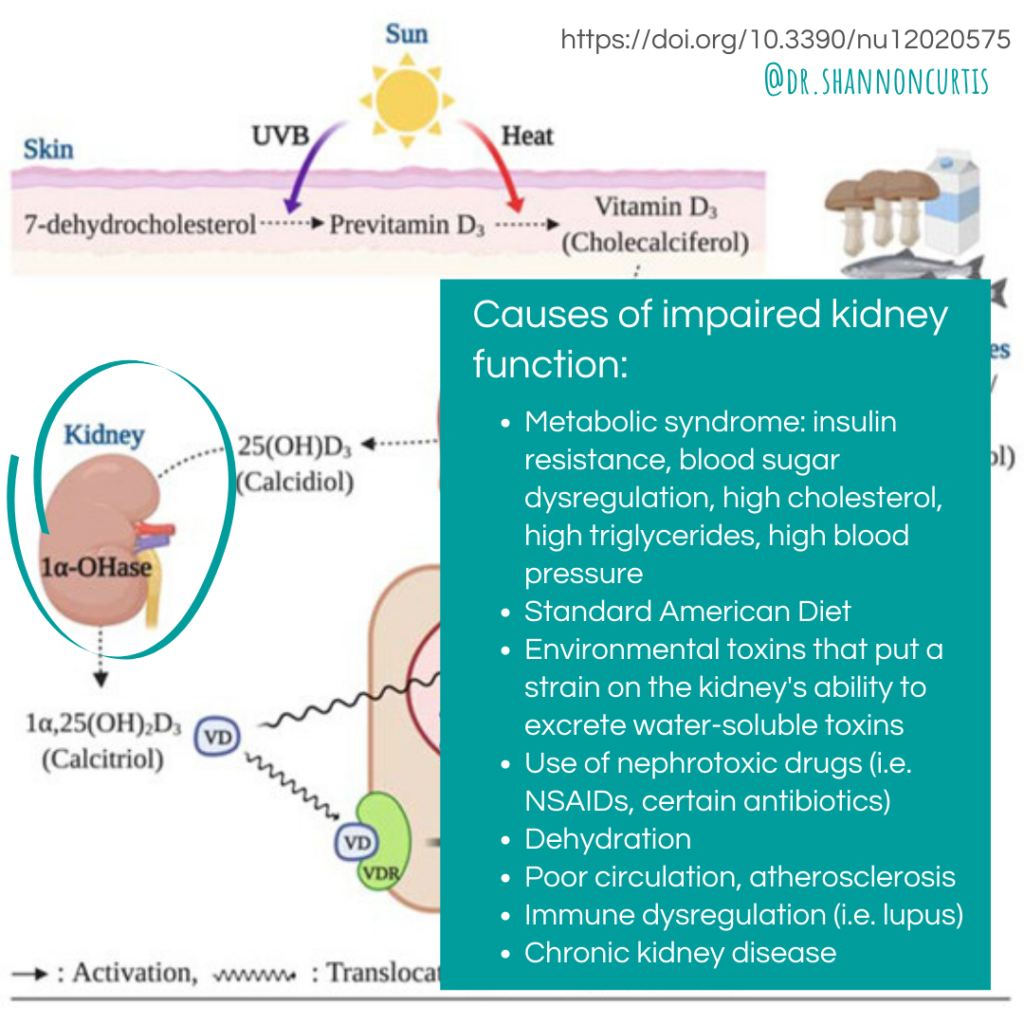
Notice that there’s quite a bit of overlap between the two, and much of it comes down to metabolic dysfunction.
Studies have shown that only 12% of American adults are metabolically healthy, meaning that they have ideal blood sugar and fat metabolism regulation, and ideal blood pressure. That means 7 in 8 people have some sort of metabolic dysfunction, and all of these people are at some degree of risk of vitamin D deficiency and immune system dysregulation! Unbelievable, right?!
Metabolic dysfunction is likely why so many people in the U.S. are considered to be vitamin D deficient, and is one of many reasons why metabolic health is so incredibly important.
Supplementing with Vitamin D
Healthy summer sun exposure–combined with healthy liver/kidney function and optimal metabolic function–means that even if you live in a cloudy climate, you can still have enough vitamin D to last you through the winter even without supplementation.
I’m not telling you not to supplement with vitamin D. Supplementation always has a time and place, just like pharmaceutical medications! Like any health intervention, you need to weigh the pros and cons for yourself and your own body, and perhaps even have a conversation with your doctor about the risks vs. benefits.
Are there risks with supplementing with vitamin D? Yes, definitely. Having too much vitamin D in your system can have negative health effects. The risks start to arise when you take 4,000 IU or more of supplemental vitamin D daily.
Symptoms of vitamin D toxicity (too much vitamin D supplementation):
- Hypercalcemia (too much calcium in your blood): kidney stones, bone pain, nausea/vomiting, weakness, confusion, fatigue, heart arrhythmias
- Arterial calcification, stiffening your arteries and predisposing you to cardiovascular disease (however, vitamin D deficiency is also associated with an increased risk of cardiovascular disease, so balance–not too much and not too little–is likely key)
So the take-home message is this: If you get regular, moderate sun exposure (even just in the summer) and make sure your metabolic health is top-notch, you’ll likely have plenty of vitamin D.
What are your thoughts? Any questions? Comment below!